Ataxia is a term for a group of disorders that affect co-ordination, balance and speech.
Spinocerebellar ataxia (SCA) is a term referring to a group of ataxias that are characterized by
degenerative changes in the cerebellum and sometimes in the spinal cord. Moreover, it is a
hereditary and progressive condition.
Presentation of SCA
There are more than 20 identified types of Spinocerebellar ataxias; SCA1, SCA2, SCA3 and SCA6
being the most common amongst all. Though each may have unique signs and symptoms, however,
in general, it is difficult to differentiate among the different types, and all are presented by problems
with movement that tend to get worse over time. Depending on the type of SCA, signs and
symptoms can develop anytime from childhood to late adulthood.
Affected people may experience some or all of the following:
- Problems with coordination and balance (ataxia)
- Uncoordinated walk (ataxic gait, also called drunkard’s gait)
- Poor hand-eye coordination
- Abnormal speech (dysarthria)
- Involuntary eye movements
- Vision problems
- Difficulty processing, learning, and remembering information
Cause of SCA
Mutations in many different genes are known to cause the different types of
spinocerebellar ataxia (SCA). For some types, the gene known to cause it has been identified, while
in others, the genetic cause is still unknown.
Spinocerebellar ataxia can be inherited in an autosomal dominant fashion. When a person with an
autosomal dominant condition has children, each child has a 50% risk to inherit the mutated copy of
the gene from the affected parent.
Diagnosis
Spinocerebellar ataxia (SCA) is often suspected when a person presents with certain signs and
symptoms, such as ataxic gait and uncoordinated hand/finger movements.
Genetic testing is the best way to confirm SCA and identify the specific type, especially when a
person also has family members with similar features.
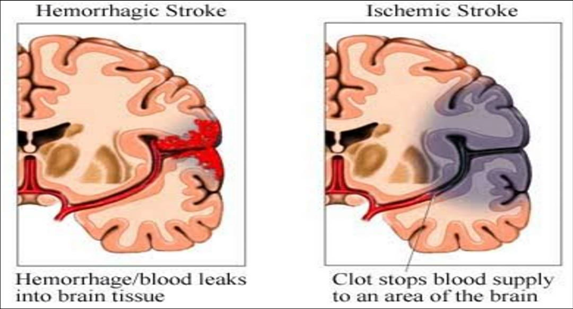
Computed tomography and/or magnetic resonance imaging (MRI scan) may be necessary to
establish a diagnosis if the genetic cause for some of the types is currently unknown
Prognosis
The long-term outlook (prognosis) for people with spinocerebellar ataxia (SCA) varies. Disease
progression and severity often depend on the type of SCA but people affected by any type of SCA
usually require a wheelchair by 10-15 years after the onset of symptoms. Many will eventually need
assistance to perform daily tasks.
Treatment
There are no known guidelines for the medical management of spinocerebellar ataxia (SCA). Each
patient requires an individualized approach according to the severity of signs and symptoms. A team
consisting of neurologist, physiotherapist, occupational therapist, speech therapist and orthotist;
working in close conjunction is often required to manage the patient with the primary goal of
keeping the patient as active as possible and improve the quality of life.
Though there are no known medications for SCA but a recent study suggests dietary
supplementation with docosahexaenoic acid (DHA) — an omega-3 fatty acid that is essential for
brain development and function — produces symptomatic improvements in patients with
spinocerebellar ataxia. Although, further research is required to establish its efficacy
Physiotherapy and Rehabilitation
Physiotherapy comprises the most essential aspect in the management of a patient with SCA. It may
not halt the disease process but it definitely helps the patient to cope up with the symptoms and
improve function to a large extent. Moreover, the earlier physiotherapy is started in the course of
the disease, the easier it becomes for the patient to manage his/her activities of daily living as well
as vocational activities.
The chief goals of physiotherapy are:
- Optimize function and improve quality of life.
- Prevention of falls by careful assessment of the reason of fall and the environment. Improving the strength and flexibility of muscles.
- Improving balance and co-ordination
- Retraining the gait (walk).
Depending on the signs, symptoms and functional limitations of each patient, a physiotherapist can
schedule a treatment plan based on two approaches:
1) Compensatory approach:-
This approach helps to improve functions of daily activities by employing few changes with
and around the patient. These may be as follows:
- A physiotherapist prescribes appropriate mobility aid such as cane, walker
or wheelchair. Also, he/she trains the patient for the usage of the aid by
incorporating strengthening programmed for specific muscles required for
the usage of mobility aid.
- He/she provides tailor-made advises on certain environmental
modifications at home or workplace of the patient such as installing ramps,
handles and bars, modifying height of bed, sofa or working chair, raising the
toilet seat etc. based on the requirements and clinical presentation.
- He/she will teach strategies to optimize the quality and ease of daily
activities.
2) Restorative approach:
Despite of SCA being a progressive condition, some symptoms show definite improvement
with regular and guided training by improving the underlying impairment. As mentioned
above, the most common impairments in SCA are incoordination, weakness of muscles,
impaired balance and ataxic gait. A physiotherapist can use various exercise methodologies
to improve each of these. These may be few or all of the below
I. Co-ordination exercises:
Frenkel exercises:
Frenkel Exercises are a series of movements of increasing difficulty performed by ataxic
patients to facilitate coordination. These are used to restore rhythmic, smooth and
coordinated movements.
The main principles of Frenkel exercises are:
- Concentration or attention
- Precision
- Repetition
Exercises can be done in four basic positions according to the level of impairment can be
used: lying, sitting, standing or walking. The exercises progress from postures of greatest
stability (lying, sitting) to postures of greatest challenge (standing, walking). As voluntary
control improves, the exercises progress to stopping and starting on command, increasing
the range and performing the same exercises with eyes closed. Concentration and repetition
are the keys to success.
II. Strength and flexibility training:
Flexibility of all major muscles should be maintained using stretching and self-stretching
techniques. The physiotherapist can design a strength training programmer which targets all
major muscle groups. He/she can employ a wide range of techniques for strengthening such
as:
- Strengthening using devices such as weight cuffs, resistance bands and tubes,
dumbbells and specially designed machines for strengthening.
- Strengthening using body weight/functional strengthening: For example; squats,
lunges, standing on one leg etc.
- Hydrotherapy
- General fitness training
III. Balance and gait training:
Though improvement in co-ordination and strength improves postural control and balance
to a large extent, but, specific techniques are commonly used by physiotherapists to train
the balance and gait.
- Somatosensory cues from the fingertips using light touch contact as a means of guidance by
the therapist can provide a powerful reference orientation while the patient is standing or
doing some activity in standing position or walking. Similarly, strong verbal cues are used in
the same manner.
- Techniques such as perturbations, reaching out to specified target, balance training on foam
mat and balance board are also the most commonly employed techniques to train balance.
- Treadmill training is also an effective method to train the gait. However, the intensity and
duration is tailor-made for each patient.
Psychosocial support
As required by patients with any neurological disorder, a strong and consistent psychosocial
support from the family members, community members as well as the rehabilitation team is
the foundation for successful rehabilitation of a patient with SCA. It is of utmost important
for the family and rehabilitation team to have a clear understanding of the disease process.
Such clarity helps to be empathetic towards the patient and also helps to formulate and
chase realistic goals for the patient. Moreover, a high level of motivational support is also
required to maintain consistency in the rehabilitation process. It is of primary importance to
maintain the individuality and dignity of the patient by the community members despite of
the functional limitations. It would really help the patient to go a long way without being
disheartened

Comments
Post a Comment